
The literal Polypharmacy definition is “many medications.” Most healthcare providers consider polypharmacy in the elderly to include patients who are 65-years of age or older that are taking five or more medications on a daily basis.
While taking five or more medications every day may be unavoidable for some people, it’s important to understand polypharmacy and the risks associated with it.
This is even more crucial when the daily pill count extends upwards of 10 medications or more each day.
Everyone should be vigilant about their health and personal wellbeing. They also need to ask physicians informed and targeted questions about the medications they are prescribed.
When used as directed, prescription medications play a vital role in improving the health and wellbeing for so many people as an antidote to what ails them.
Unfortunately, when medication use leads to polypharmacy, the cure can quickly become the disease.
What is Polypharmacy in the Elderly?
There’s no getting around the fact that drug therapy is effective at slowing and preventing the progression of many diseases.
However, the risks due to adverse drug interactions, patients misusing prescriptions, and other issues are all essential factors that must be considered.
People 65 and older are the demographic using the highest number of prescription medications.
Research shows that 50 percent of elderly patients are taking at least one unnecessary drug.
Polypharmacy in the elderly can be broken down into three categories:
1. Excessive Polypharmacy
Taking 10 or more drugs regularly is known as excessive polypharmacy.
2. Polypharmacy
Using five to 10 medications is the basic definition of polypharmacy.
3. Absence of Polypharmacy
Only taking four medications or less is considered to be an absence of polypharmacy.
Taking a high number of different medications daily increases the risk for health complications.
There can be a danger of what is referred to as prescription cascades. This occurs when additional drugs are prescribed to treat to the adverse interactions of other prescriptions.
In some of these cases, a false diagnosis might mistakenly be made about an issue that is simply an adverse reaction from one or more medications.
When a patient is using a high number of medications, the likelihood for mistakes increases. Mistakes might be patient-related when they live in their own home.
In assisted living facilities where medications are dispensed to residents, the chance that caregivers might make a medication error also increases. This is especially problematic when patients are prescribed new meds, or taken off old ones.
It’s important to note that Polypharmacy should not be confused with polysubstance abuse. This often involves recreationally taking more than one drug at a time for the “high” produced from mixing them.
Ways of Reducing Polypharmacy in the Elderly
Medically risky polypharmacy in the elderly occurs when a patient takes one or more medications that are not necessary.
When a medication is no longer needed, it offers an opportunity to reduce the number of drugs a person is using and discontinue the use of one or several prescriptions.
Reasons to discontinue a medication include:
1. A combination of several drugs, or even just one of the medications, causes unacceptable issues or puts the person at a high risk for adverse interactions, such as serotonin syndrome symptoms.
2. One or more of the medications does not successfully achieve its therapeutic goal.
3. The drug does not work as intended like it once did, or additional new medications counteract the effects.
4. There is no evidence-based indication for prescribing the drug.
5. The prescribed dose is unnecessarily high.
6. An elderly patient is either unable or unwilling to take the medication as prescribed.
Polypharmacy Statistics
In 2019, the U.S. Census Bureau estimated that 54 million Americans were aged 65 or older.
Where polypharmacy in the elderly is concerned, this is the demographic segment of the population that is most at risk.
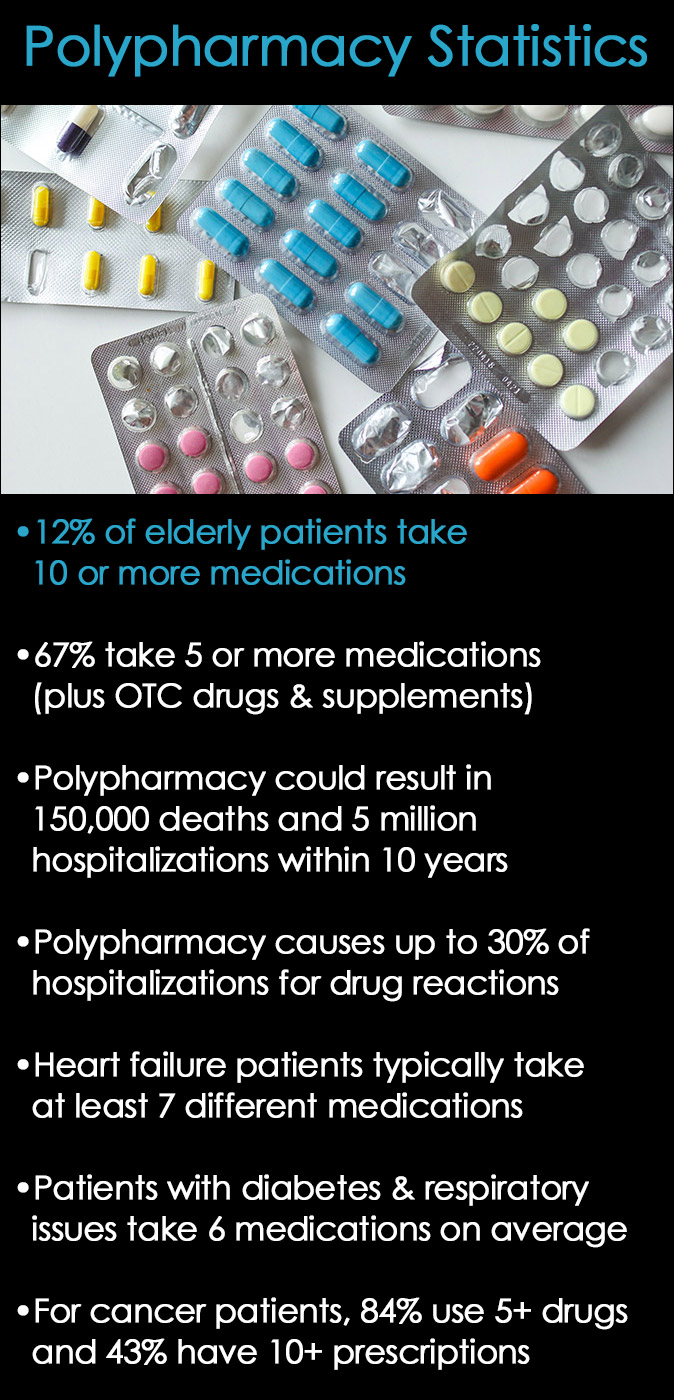
Recent Polypharmacy Statistics
Cureatr medication management solutions published the following data regarding polypharmacy statistics.
- Approximately 12 percent of the elderly population is taking 10 or more medications
- An estimated 67 percent of older Americans take five or more medications including over-the-counter drugs and supplements, which may interfere with prescribed drugs, according to a study published in JAMA Internal Medicine
- Research published in 2019 suggested that polypharmacy could result in 150,000 deaths and nearly 5 million hospitalizations over the next decade
- It’s estimated between 10 to 30 percent of all hospitalizations for adverse drug reactions can be attributed to polypharmacy
- Patients suffering from heart failure are typically taking at least seven different medications
- Elderly patients with type 2 diabetes, respiratory issues, and coronary heart disease, on average, take about six medications
- Considering elderly polypharmacy patients with cancer, 84 percent use five or more drugs, and 43 percent have 10 or more prescriptions
It should be mentioned that when properly managed, polypharmacy is not necessarily a bad thing.
Data has shown that 26 percent of patients in nursing homes who were prescribed several medications following a heart attack were less likely to die within 90 days than patients prescribed just one medication.
Common Polypharmacy Risk Factors
There are quite a few reasons that polypharmacy can unwittingly become part of a person’s daily routine.
One reason that is inescapable is due to age. As people get older, they tend to experience poor health issues and require medications to alleviate pain or address other circumstances related to aging.
While medications are helpful for treating a variety of conditions, many cause negative side effects that contribute to other health issues.
Typical Medication Side Effects include:
- Headaches
- Nausea
- Constipation
- Diarrhea
- Weight loss or weight gain
- Insomnia
- Drowsiness
- Cognitive impairment
- Dizziness that leads to falls
- Memory problems
- Substance-induced disorders
When side effects arise from talking any type of medication, it’s not uncommon for doctors to prescribe an additional one to overcome the symptoms. It’s easy for this cycle to continue as new prescriptions are added to the mix.
Another frequent issue that promotes polypharmacy involves multiple chronic conditions that require drug treatment, such as cancer, Alzheimer’s, or other age-related diseases and disorders.
An extremely familiar, though rarely discussed concern is self-medication, either with over-the-counter drugs, alcohol, or illicit drugs.
Self-medicating is particularly dangerous because not only can it lead to dangerous drug interactions, but it may also lead to issues of addiction or a substance use disorder that requires treatment at a rehab facility.
It’s not unusual for patients dependent on certain medications to also use several different doctors and pharmacies to game the system (doctor shopping), or to use medications that were originally prescribed to friends and family.
Other polypharmacy risk factors can include:
- Doctors who have too many patients or an unsustainable workload
- Patients who withhold information from their doctor
- Physicians who poorly communicate with their patients
- Doctors who lack sufficient education or competency about a particular illness or condition may prescribe an inappropriate medication or dosage level
- Ineffective transition of care, either from physician to physician, from hospital to nursing home, or from a hospital to a caregiver
How Can Older Adults Avoid Polypharmacy?
Understanding how to prevent polypharmacy in the elderly requires education and vigilance, not just on the part of physicians and health care workers, but also on the part of the patients and their loved ones.
There are a number of strategies to improve polypharmacy statistics and the well-being of older adults who require daily prescriptions.
It’s vital for patients and family members to keep a comprehensive list of all medications, including over-the-counter meds and supplements. This information should be disclosed to all examining physicians on a regular basis.
It’s necessary to mention non-prescription medications that are used periodically, such as Triple C (Coricidin, cough, and cold) because they can cause an unhealthy reaction when mixed with certain prescription drugs.
Any changes in health while taking new prescriptions should be clearly communicated to the prescribing doctor.
Patients and their caretakers should know the purpose of each medication, its potential side effects, adverse interactions with other medications, and the expiration date of all prescriptions.
Some prescription drugs like Gabapentin can amplify the effects of other drugs or medications and increase the potency of all being taken at the same time.
In addition, following directions and taking medications as they are prescribed is crucial. If any negative issues arise, from adverse interactions, to dependency or substance misuse, do not ignore it.
There is absolutely no shame in seeking help for health or dependence issues that developed as a result of polypharmacy.
Deprescribing Medications
Finally, there is a recent trend in “deprescribing medications” for patients who are either taking too many daily prescriptions, or those who have suffered with negative health consequences due to medication conflicts.
It’s not unusual for people to become lethargic or struggle with cognitive delays because of too many medications that contradict each other.
The website, Deprescribing.org, provides information, research, and resources for understanding ways to work with physicians to prune away risky or unnecessary medications that have led to polypharmacy for the optimal health of the patient.
Related Posts
- Alcoholism Statistics and Facts
When asked what they think is the most heavily abused drug in the United States,…
- A Month of Awareness: National Recovery Month + Suicide Prevention Month
September is National Recovery Month and National Suicide Prevention Month to create awareness about each…
- National Impaired Driving Prevention Month in December
December is recognized as National Impaired Driving Prevention Month. During the holiday month, it’s an…
